As rates of Ebola infection fall in Guinea, Liberia and Sierra Leone, planning has begun on how to rebuild public health systems and learn lessons from the outbreak.
Nobody is declaring victory yet. But in Sierra Leone, the worst-affected country, there were 117 new confirmed cases reported in the week to 18 January, the latest statistics available, compared with 184 the previous week and 248 the week before that. Guinea halved its cases in the week to 18 January – down to 20 – and Liberia held steady at eight.
The epidemic is not over until there are zero cases over two incubation periods – the equivalent of 42 days. “It’s like being only a little bit pregnant – there’s no such thing as a little Ebola. We have to get to zero, there can be no reservoirs of Ebola,” Margaret Harris, spokesperson of the World Health Organisation (WHO), told IRIN.
But after 21 724 cases and 8 641 deaths in nine countries since the epidemic began in Guinea last year, there is some light. And health workers are already starting to look at what’s next. “Right now important meetings are going on in each country to work out what needs to be done to rebuild – in some significant respects to build health systems almost anew – and to build back better,” said Harris.
A European Union donor conference is due at the beginning of March in Brussels. “What we want to see as a country is a resilient health system that can withstand shocks,” Liberia’s Assistant Health Minister Tolbert Nyenswah told IRIN. “Our plan [to be presented in Brussels] will be finalised by the end of February. It will be well costed with tangible goals.”
Ebola tested the public health systems in the three West African countries to near destruction – most places in the world would have also struggled. But where the three failed was at the basic “nitty-gritty” level of “standard surveillance, testing and monitoring, the containment of cases, the bread and butter of public health”, said Adia Benton, a social anthropologist at Brown University in Rhode Island.
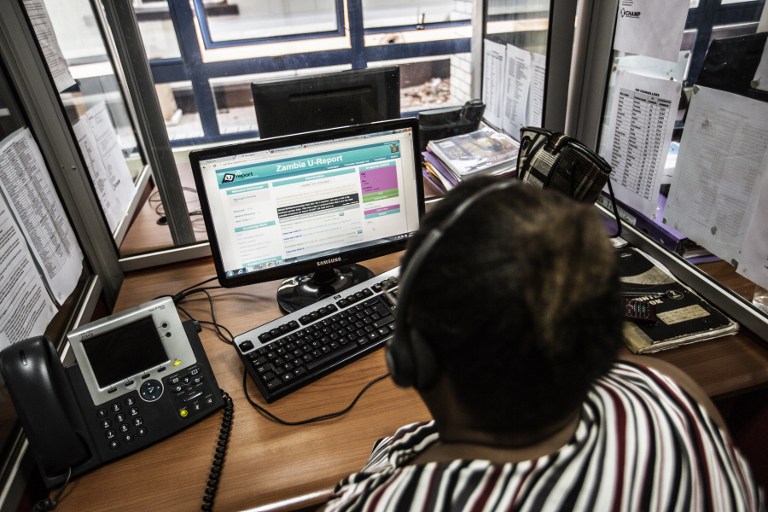
Citizen and state
A successful malaria campaign in Sierra Leone last week, which reached 2.5 million people, and a planned polio and measles vaccination programme in Liberia, are positive signs for the health services. But the list of necessary reforms is long: stronger surveillance; healthcare that will work after the international partners leave; access to affordable services. The list must also embrace longer-term structural changes, including the relationship between citizen and state.
According to Antonio Vigilante, Deputy Special Representative for the Consolidation of Democractic Governance in the UN Mission in Liberia, and Resident Coordinator, “there is a golden opportunity to have a different start, to have a more balanced development that leaves outcomes in the hands of the people. It’s a very delicate stage, full of opportunities, which should not be missed.”
Liberia is one of the world’s poorest countries and Ebola has been a tragic addition to the burden. It has destroyed livelihoods; already dizzying rates of unemployment have worsened; and food prices have soared. Both rural and urban communities are suffering.
Vigilante is worried the economic impact of Ebola, and the interruption of immunisation and reproductive health services during the crisis, could put more people at risk than the virus itself did. “A number of [social protection] measures in the recovery phase would need to be universal,” he said. One example would be if Liberia scaled up its pilot Social Transfer Programme, launched in 2009, to provide just US$40 per year to two million children. There would be sizeable “knock on effects on local markets and entrepreneurship” at minimal cost, according to the Washington-based Centre for Global Development.
Schools are due to re-open on 2 February in Liberia, and a strong case could be made for a universal school feeding programme to attract and retain children in class. “Even before Ebola many children were out of school,” UNICEF spokesman in Liberia, Rukshan Ratnam, noted.
Money matters
But will the donors come to the party? Donors pledged $1.5 billion to a UN coordinated appeal for Ebola last year, but $500 million is still unpaid. “If we cannot close that funding gap we will snatch defeat from the jaws of victory. It’s as simple as that,” Bruce Aylward, WHO assistant director-general in charge of the Ebola response, told reporters on January 23.
Wasted dollars can be expected in a crisis when the priority is effectiveness – stopping the outbreak – rather than efficiency in how the money is spent. That equation will change if Ebola does not come roaring back with the rains in April, and donors begin to look at competing needs.
There is potential to re-purpose Ebola infrastructure – some of it now idle with a glut in treatment facilities – if donors are willing to be flexible, said Vigilante. Laboratories used for testing could be incorporated into national laboratory services; some of the more permanent treatment units could be re-launched as community-based health facilities; contact tracers could be used as community mobilisers.
“We certainly lost staff as a result of Ebola. But the converse of that is there was a very rapid upskilling as people were trained to work in the treatment units or as contact tracers. It’s a group we should build on,” said Harris. “It’s really important we don’t lose them in the transition to a normal service.”
Local heroes
Among the lessons learned across the region has been the importance of consulting, engaging and empowering local communities: their lack of trust in central government was a major handicap in tackling the epidemic. “Community, community, community. Engagement, engagement, engagement,” said Harris. “We need to listen more. We need to do a lot of work with sociologists and anthropologists.”
Liberia in particular has a highly centralised system of government, but local communities have emerged as critical players in the response with a new can-do attitude. “People given a chance can do a fantastic job,” said Vigilante.
Obinna Anyadike, Editor-at-Large for IRIN